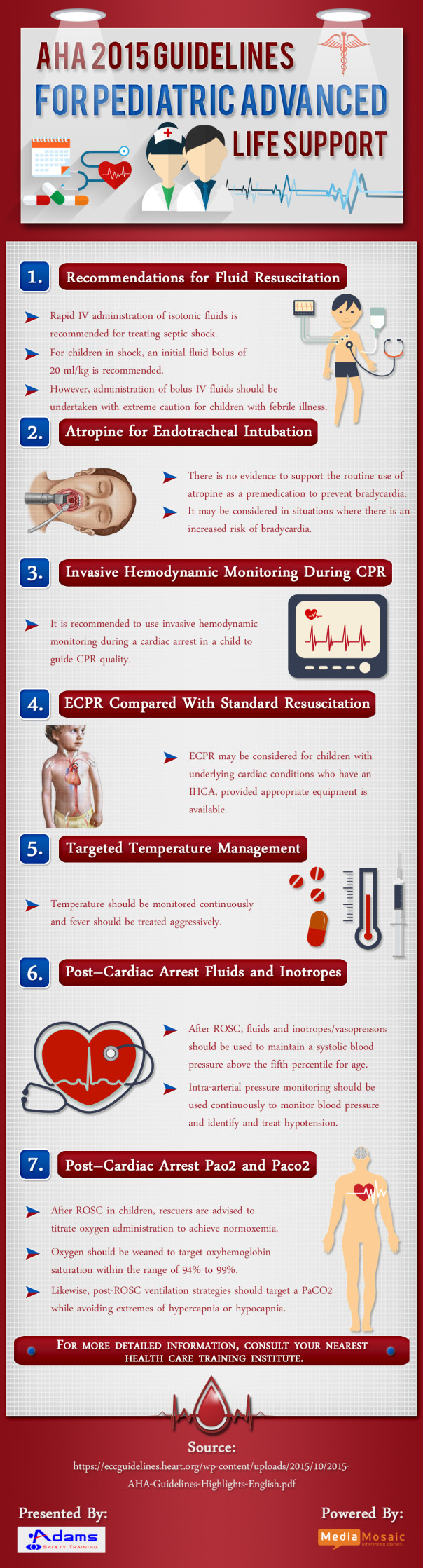
The given Infographic summarizes the updated guidelines for pediatric life support issued by AHA. Earlier in Oct’2015 AHA released the updated CPR guidelines.
New information or updates are provided about fluid resuscitation in febrile illness, atropine use before tracheal intubation, use of Amiodarone and Lidocaine in shock-refractory VF/pVT, TTM after resuscitation from cardiac arrest in infants and children, and post–cardiac arrest management of blood pressure.
Atropine for Endotracheal Intubation: There is no evidence to support the routine use of atropine as a premedication to prevent bradycardia in emergency pediatric intubations. It may be considered in situations where there is an increased risk of bradycardia. There is no evidence to support a minimum dose of atropine when used as a premedication for emergency intubation.
Invasive Hemodynamic Monitoring during CPR: If invasive hemodynamic monitoring is in place at the time of a cardiac arrest in a child, it may be reasonable to use it to guide CPR quality.
Targeted Temperature Management: For children who are comatose in the first several days after cardiac arrest (in-hospital or out-of-hospital), temperature should be monitored continuously and fever should be treated aggressively. For comatose children resuscitated from OHCA, it is reasonable for caretakers to maintain either 5 days of normothermia (36°C to 37.5°C) or 2 days of initial continuous hypothermia (32°C to 34°C) followed by 3 days of normothermia. For children remaining comatose after IHCA, there are insufficient data to recommend hypothermia over normothermia.
Post–Cardiac Arrest Fluids and Inotropes: After ROSC, fluids and inotropes/vasopressors should be used to maintain a systolic blood pressure above the fifth percentile for age. Intra-arterial pressure monitoring should be used to continuously monitor blood pressure and identify and treat hypotension.
For more guidelines go through the Infographic below: